
While the media often focuses on emotional side effects, the single most significant, quantifiable, and life-threatening risk of exogenous testosterone use is the resultant increase in red blood cells (RBC), a condition known as secondary Polycythemia or Erythrocytosis.
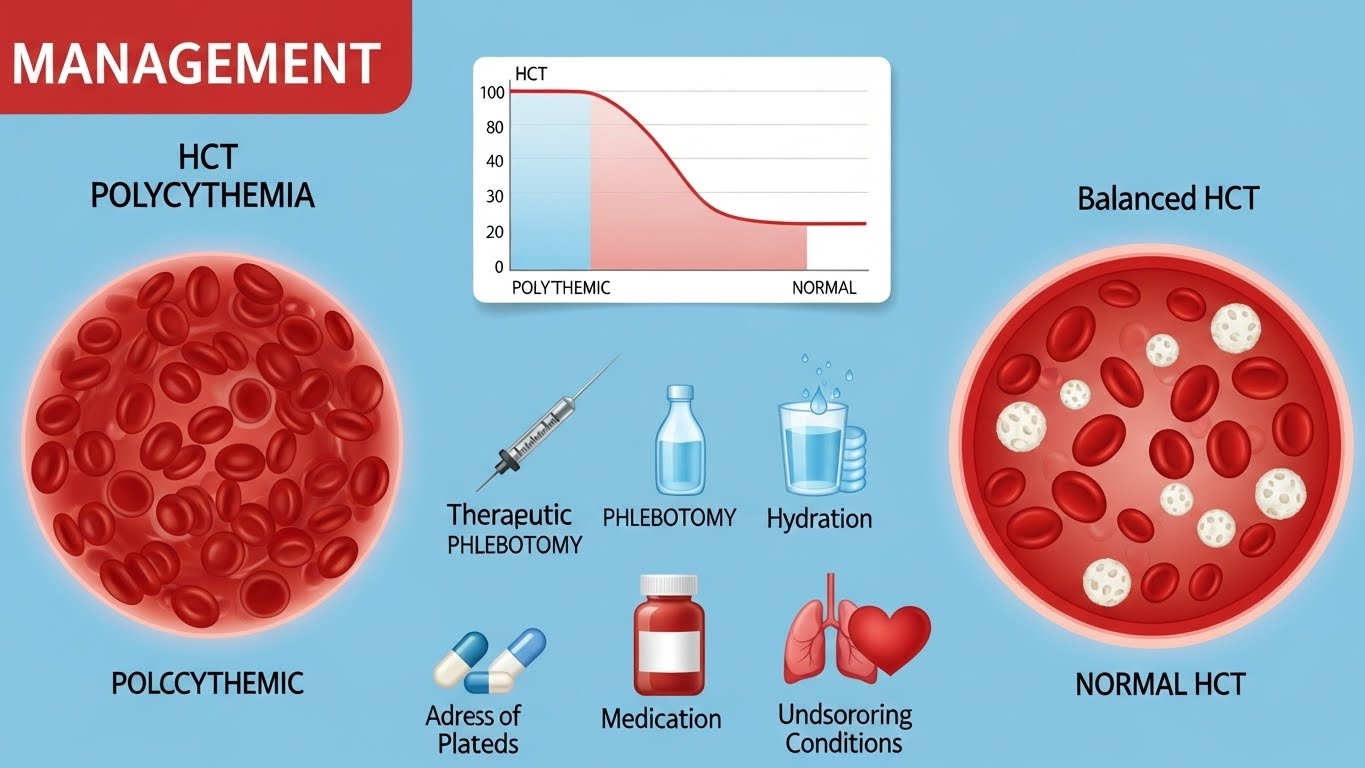
Testosterone acts as a stimulus for Erythropoiesis (the production of RBCs). As the number of RBCs increases, the blood becomes thicker (more viscous). This state is measured by Hematocrit (HCT), which is the percentage of your total blood volume occupied by RBCs.
Learn more about testosterone with our ultimate Canadian TRT guide
Clinical guidelines are extremely clear on the threshold for intervention. Your personal QC must strictly adhere to these limits.
|
Condition |
HCT Level |
Action Required |
|
Normal Male Range |
40%–50% |
Continue monitoring, no action needed. |
|
Alert/Pre-Intervention |
50%–52% |
Requires increased hydration, dosage reduction, and immediate retesting. |
|
Intervention Zone |
52% and above |
Mandatory intervention. Clinical guidelines dictate either stopping T use or performing therapeutic phlebotomy. |
Concentration variability, common with grey-market products, is a major factor. If your Test C is dosed infrequently (e.g., every 10–14 days), the high peak concentration causes a massive, temporary spike in RBC production. The recommended shift to minimum twice-weekly dosing minimizes these peaks and is the first line of defense against HCT creep.
Before resorting to blood removal, the first steps involve dosage and lifestyle adjustments to allow the body to naturally manage the red blood cell (RBC) count.
If you are injecting less than twice weekly, switch to a smaller, more frequent injection schedule (e.g., 50mg three times per week, instead of 150mg once per week). By keeping the serum levels more stable and flattening the hormonal peak, you reduce the strong stimulus on the bone marrow to produce RBCs.
Dehydration can artificially elevate your HCT reading, as the blood plasma volume decreases. Ensure high water intake, especially in the 24 hours before a blood draw, to ensure the reading is accurate. High-intensity exercise can also temporarily skew the number upwards due to fluid loss.
If your HCT rises above 50% and remains there despite improved dosing frequency, you must reduce your overall weekly dosage. Prioritize long-term safety over maximizing the immediate concentration.
When HCT remains at or above 52%, Therapeutic Phlebotomy (blood donation/removal) becomes a mandatory procedure. This physically removes the excess red blood cells, instantly lowering viscosity and reducing clot risk.
This is a medical procedure where approximately 450ml to 500ml of blood is safely drawn from a vein, identical to the process of standard blood donation.
Self-monitoring Polycythemia requires a dedicated QC cycle: